For 10 years I have been a nurse in the multidisciplinary I.C.U. at M.G.H. Boston, and while we have encountered countless tragedies before, none have challenged us — or me — like the COVID-19 pandemic. We opened this 18-bed unit in 2011 and since its opening, it has tended to attract some of the younger nurses who are looking to learn and be part of an innovative, hands-on, dedicated team. I carry a lot of pride in my team and in this unit and I want people to know that we will provide the best care possible. I also want my nurses to feel supported that they have the skills necessary to take care of these critically ill patients.
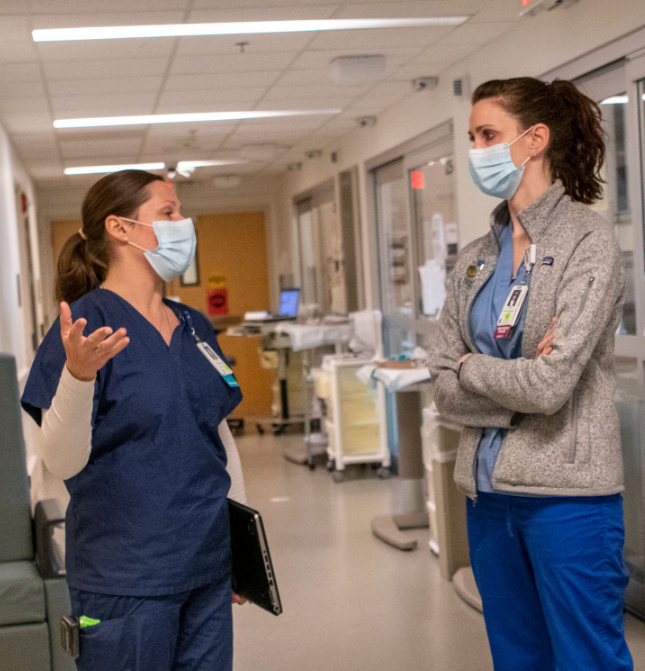
My current role is that of nurse educator and practice specialist, and I also help nurses in the care of patients at the bedside. Even in pre-pandemic times, I put a lot of pressure on my shoulders to be a leader to my team and to provide simultaneous support to patients and nurses alike. When the pandemic hit, the pressure of all of these roles increased tenfold. These patients were so different — they were so incredibly sick and were not getting any better. At the same time, our team had to become experts in this novel virus overnight. Some new nurses were still learning to take care of critically ill patients, so I had to keep my leadership hat on at all times while remaining present to provide support at the bedside to learn and better understand what was happening with this virus and its devastating effects on our patients. I had to be open and available to my team at all times while personally dealing with and adjusting to the uncertainty of the situation, which was far more challenging than I could have ever anticipated.
As a leader, I try to push my nurses to take time for themselves, even if it’s just taking a quick break to go outside and get a breath of fresh air. I know the importance of self-care because I learned the hard way. During the Boston Marathon bombing in 2013, I was a nurse at the bedside caring for one of the three victims on our unit. I took on a lot of the emotions of the victims’ families like my own and had trouble separating myself from the tragedy that occurred. Following the bombing, people around me were telling me that I was starting to fade. I was exhausted and depleted and it was in that moment of darkness that I turned to running, which became one of the coping strategies I found that helped me to process some of the trauma I was experiencing. I also sought out individual therapy through our employee assistance program because I felt like I was spiraling and losing my ability to get out of bed every day. Both therapy and running saved my career. Every pounding of my foot as I ran pounded out my stress and released that which I could not control.
I can relate the experience of the pandemic to how I felt after the bombing. I knew that if I didn’t find an outlet and take that time for myself, I was heading towards a really bad place. I know first-hand how it felt after experiencing such a tragedy to completely become a shell of a human being with no desire to feel anything but sadness for my patient and his family. I saw this happening with my nurses as they stood in for the patient’s family and held the hands of a patient dying of COVID. I wanted to ensure that my nurses didn’t need to hit rock bottom to start taking care of themselves. I wanted to teach them a better way. Being an I.C.U. nurse is already such a challenging and demanding job — it’s essential to create boundaries that allow you to process your experiences and protect your mental health.
The challenge is that we are very much still living the pandemic. With the bombing, once I could finally process it, I could help other people, but it’s hard for me to do that now because it has not stopped — I have not had the time to process it or learn from it in the way I wish I could. In addition, I injured myself in the early days of the pandemic, so I have not even had the outlet of running to turn to. Dealing with an injury during this time hasn’t been easy, but I have tried to accept that maybe life is calling me to heal my trauma in a different way. While last time I used running to initiate the process, this time I am using my mind.
Whether it is breathing exercises or meditation, I have tried to build a mindset that is forward-thinking and hopeful, which is all very new to me. I have also taken the opportunity to participate in the Resiliency Rounds offered through my hospital, which offers our teams the chance to share our experiences with executive leadership in response to open-ended questions. I have also noticed how important my days off are for me to reset so especially on the days I feel the anxiety creeping in, I’ve pushed myself to read a book, turn my head off, and give myself that time and space to rest and recharge. While there hasn’t been a silver bullet to help me process in real-time the trauma we are experiencing, these little moments of self-care have helped to better focus on the hopeful future ahead, knowing that we are “one day closer to the end” — this is what I told my staff since the day that I recognized that we were about to be tested on just how strong and resilient we were as a team.