This piece was first posted on Substack. To comment, please go there.
Readers of this column will recognize several familiar themes. One of them is that the world is not straightforward, and interesting answers are seldom simple. I have written previously about how core to our thinking about health should be a capacity to engage with ambiguity and issues which do not always neatly resolve. This has never been truer than when it comes to the issue of national borders in the context of pandemics. Borders and migration have long been some of the most fraught terrain in our current political debate. The issues elicit strong feelings on all sides—whether one favors maximally exclusive national boundaries or something akin to open borders. The conversation about borders becomes even more complicated in the context of infectious disease outbreaks.
At the core of the issue are two contradictory, yet equally true, realities.
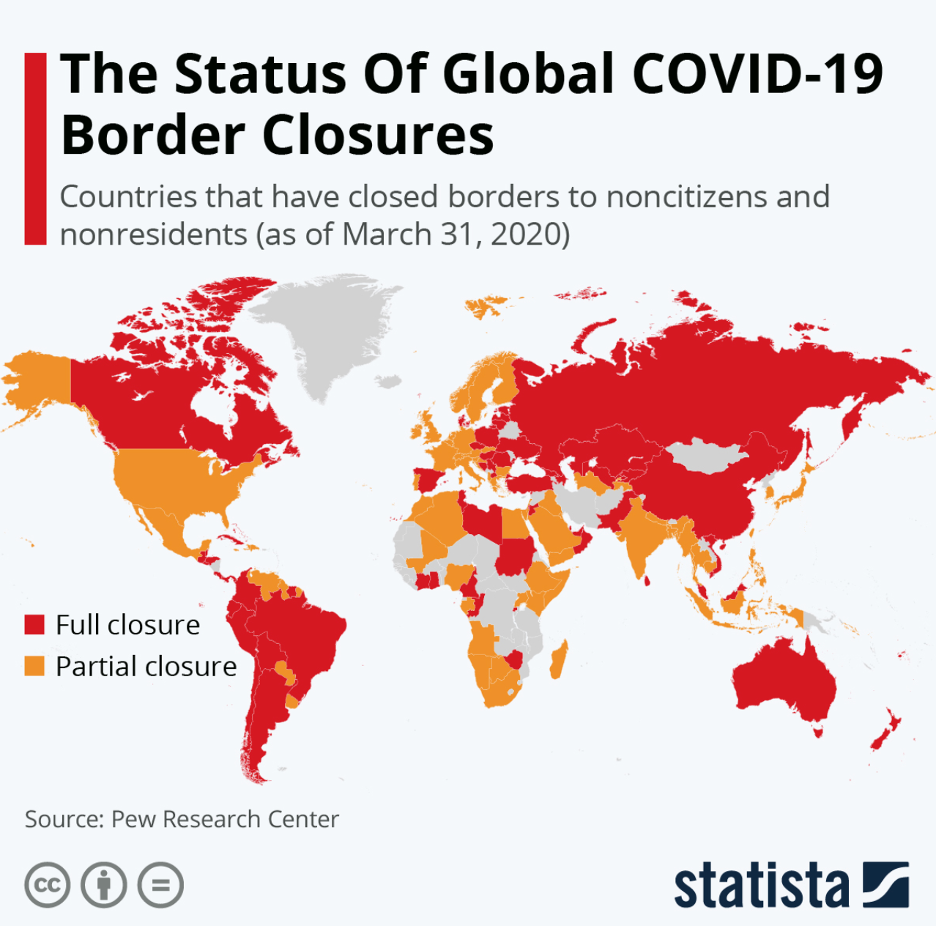
First, pandemics expose the fundamental interconnectedness of health. It is the case that outbreaks will spread without heed to the artificial lines on maps we call “borders.” With that in mind, borders can play a role in containing outbreaks and closing national borders as early and tightly as possible during an outbreak can, combined with aggressive in-country testing and tracing, help to protect populations from emergent world-wide contagion. The figure below reflects the world’s dawning appreciation of this, showing the state of border restrictions early in the COVID-19 pandemic.
The second reality is that borders, by their very nature, represent lines drawn, the demarcation of “us” and “them,” which, when drawn harder (i.e., when closed), quickly pave the way for hardening of nationalistic impulses. Measures to restrict travel, even if necessary, can fuel xenophobic attitudes, as a disease originating in a certain region gets conflated with the people living there, and the work of shutting out contagion seems to become the work of shutting out these populations. This can lead to racism and bigotry, particularly when it is not handled in a politically responsible way. In an increasingly mobile world, border closures can also separate families, friends, colleagues, and the social supports that we know promote health and make for a full life. This does not even speak of the economic consequences of closures, which may disproportionately affect people with fewer resources. Closing these lines drawn can create division and rewire our communities.
Which raises the question: are border closures worth it? When might they be? When might they not?
A core imperative of public health is to work towards a world without the divides of which borders can be physical and symbolic representations. At the same time, public health’s pursuit of this goal should not stop us from acting decisively, particularly at the start of a crisis, when border controls could play a key role in stopping the spread of disease and time is of the essence. Conversations about how we can mitigate xenophobia and advance a more open world are central to the work of public health—to neglect these conversations would be to abrogate our mission. But if such conversations cause us to lose a week or even a month at the start of an outbreak, when swift border closures can make a key difference—as they did during COVID-19 in places like New Zealand and Taiwan—this, too, would be to neglect our core responsibilities.
The World Health Organization’s changing approach to border closure during the COVID-19 pandemic represents a confluence of contradictory good intentions and the conflict between different, equally important, imperatives. The WHO was resistant to suggesting border closures at the outset of COVID-19. In early 2020, WHO Director-General Tedros Adhanom Ghebreyesus, informed by the 2005 International Health Regulations, spoke out against border closures, saying “There is no reason for measures that unnecessarily interfere with international travel and trade.” This reflected an understanding that health is more than just the absence of viral threats, that the material resources generated by trade, and the flow of people (including the health care workers so central to mitigating an outbreak) are also core to supporting health at all times, but particularly in moments of crisis. The WHO came under substantial criticism for this position and eventually somewhat changed its position on border closures as the scope of the pandemic became apparent.
What do we learn from this moment? Three thoughts that I think can inform our evolving thinking on the issue, reflecting the array of complexities involved in grappling with the challenges of borders.
First, the context within which we are thinking about borders being open or closed matters quite a bit. There was, during COVID-19, the unique factor of President Trump; his long history of xenophobia ensured that when he eventually called for border closures, the issue would become immediately enmeshed in the broader culture war. It was difficult, perhaps impossible, to have a good-faith conversation about the necessity of restricting travel into the US when the person in charge of executing such a policy was so deeply compromised on the issue. This speaks to the importance of having a conversation about borders and immigration that rejects xenophobic rhetoric, in which political leaders take care not to fan the flames of hate. Aside from the moral imperative of this, when the conversation about borders is rendered toxic by bad-faith actors who engage irresponsibly with the issue, it becomes far more difficult to have a pragmatic discussion about it, with all its ambiguities and tradeoffs.
Second, we are living in a time when the very notion of borders is being called into question. There is growing movement in progressive circles to liberalize borders, with some seeing them as a racist colonial artifact, and open borders as reparations for past injustice. This poses a kind of left-wing counterpoint to the bellicose nationalism and xenophobia which can exist on the right. These political arguments—both of which centrally engage with the question of what borders mean—complicate our choices about what borders should do in the context of pandemics. It is important to note that public health is not neutral in this debate. Our work is based on an understanding of the fundamental interconnectedness of health, on a rejection of xenophobia and hate, and on an appreciation of the role of past injustice in shaping present sickness. For these reasons, engaging with the left-right debate over borders in a time of pandemics is not a matter of carefully splitting the difference, but of taking the progressive position in support of a philosophy that unites rather than divides.
Third, when borders are closed, it becomes difficult to know when to reopen them, which can lead to complications in our broader pandemic response. Say that early border closures do indeed succeed in saving a country from the worst of an initial outbreak, yet the pandemic rages unchecked in other countries that were not so effective in their response. When, then, should the country in question open its borders and risk letting in the virus? Must it wait until the entire world gets the pandemic under control? Or might an earlier reopening be feasible under the right conditions? The answers to these questions are not obvious. Then there are the unique challenges which can come with success. If a country manages to maintain some level of normalcy amidst a global pandemic by shutting its borders, it can be easy for the population to feel it has “beaten” the crisis, which can lead to complacency, backsliding on the very protective measures which support this success, and, perhaps worst of all, less urgency to embrace vaccines, out of a belief that they are perhaps less-than-necessary in a context of low case rates. In Australia, for example, the current pace-setter for border closures, vaccination lags substantially behind other high-income countries, with just about 15 percent of adults fully vaccinated. This is likely in no small part because the population is not particularly motivated to get vaccinated due to its early success in guarding against COVID-19. This potential tradeoff, as well as the social and economic effects of indefinite border closures, make it necessary to carefully weigh the costs/benefits of taking such a step, particularly over the longer-term. It means aiming to strike a balance, similar to that of the moral-empiric balance I addressed in a prior column, in any action we take to support health during a pandemic.
Given these factors, it strikes me that public health has a first-and-foremost responsibility to advance a unifying vision of health based on the reality of our connections to each other, while at the same time meeting the practical demands of the moment, which means recognizing the utility of borders in containing outbreaks. Failing to advance a unifying vision, failing to reject xenophobia and hate, and countenancing arbitrary, destructive divides creates a context for poor health which ultimately informs a vulnerability to pandemics. For this reason, border closures should not be used lightly in the context of supporting health. That is not the same as saying that they should be used as a last resort, because, in the context of a pandemic, the early use of border closures is the time when they can be most effective. When not used early and decisively, they can indeed be ineffective and even destructive, serving little purpose but to block the flow of people and supplies and fuel xenophobic resentments. Even in places where early shutdowns were most effective during COVID-19—such as Taiwan—diminishing returns set in as the pandemic continued. It is also true that early shutdowns are most effective when they take place in the proper context, one which includes aggressive testing and tracing and the presence of political leadership willing to use travel restrictions in a measured way.
A useful historical parallel for this extraordinary-times-calling-for-extraordinary-measures perspective, comes not from the history of pandemics, but from the American Civil War. During the war, President Lincoln suspended the right of habeas corpus. He did so narrowly, taking pains to avoid overreach, and making it clear that he did so only in response to an unprecedented national emergency. Seen in isolation, the suspension of so fundamental a right is clearly disharmonious with core Constitutional principles (although the Constitution does provide for suspending the right in cases of “rebellion or invasion”). It is also easy to see how a less responsible leader might have approached such a move in ways that seriously threatened the rule of law in the country. Yet in the context of the emergency of the Civil War, and Lincoln’s own restraint, a case could be made for the step’s necessity—even for the irresponsibility of failing to take it in defense of the broader integrity of the Union. This is not to deny the undesirability of such a step, much less to argue that suspending habeas corpus is something to be generally embraced. It is just to say that it is not inconsistent with a philosophy which deplores such measures to accept that, in certain unique cases, the needs of the greater good create an opening—indeed, an imperative—for the decisive, if circumscribed, taking of these steps.
It is likewise true that public health can embrace the pursuit of a world without borders, while at the same time allowing ourselves the freedom to act pragmatically when crisis strikes, even when this means making use of something we may wish did not exist—namely, sharply-defined national boundaries. That we might keep such a tool in our armamentarium can seem like a contradiction of our broader embrace of a world as free of division as we can make it, and perhaps it is. Yet we need not fear contradiction, and it is precisely the presence of such tension that suggests our engagement this issue is based on the complex realities of life rather than on the ideological shibboleths which can so easily become a counterproductive influence on our efforts.


