or…Let’s laugh: Temper and Belly Laughs……Not Just for Toddlers Anymore:
How feelings can be beneficial including how they can get in the way
Here’s a confession: I like sounds……(other people laughing)
I like eating….. (until I am just the right amount full……)
and sometimes, I communicate with a glance (or a pretty loud drop. I’m fairly clumsy)
Here’s something we probably have in common:
(1) We show emotions: a) we tend to talk about things we like, b) we like to eat a little or not too much, depending on the way
Or…….
(2) The thing we have most in common is that the emotions you tend to feel tend to be less extreme.
A person who is having a feeling they are trying not to communicate may:
a) shift when they are frustrated to indicate discomfort
b) sigh, but just a little
C) put on their sunglasses/listening device
(common denominator: does not like to show emotion/tends to avoid attention but actually may want it)
As I am writing, I’m thinking about some dudes I know who have some difficulties with regulating themselves, and I can remember some woman friends who indicate it by talking a titch less. I’m thinking about times that I keep talking when I know I should probably talk less, and about other time when I talk more.
Investigate!
Here’s an example of something that could also be something that shows emotion:
1. drawing more
2. getting fairly angry and
3. understanding what someone else’s people or things might mean. An example of this might be someone who likes to draw to demonstrate emotion.
They might draw an entire picture when feeling a little frustrated. Another option is utilizing that same energy they have and are trying to harness by thinking up a story or looking out a window.
If the person reading this is the ‘emotions tend to run high’ type, (number one) they might
1. miss sleep or
2. have more temper responses than others, which includes ways they show it. Some of the behaviors could include:
1. Becoming quite agitated, or upset. 2. be a person reading this who BBelow are some examples of regulation/dysregulation.
‘He gets really dysregulated when his schedule changes. His sleep schedule gets messed up, he won’t go to bed on time and then I’m tired. He is a really hard to manage kid’.
‘She was really dysregulated when she came home from her visit with her mom, and back to her foster parents’ home. She comes home so upset after she sees her mom once a week and her mom has to go back to the apartment that she’ll cry for hours. I hope her mom gets a place big enough for her children soon’.
‘He just completely flew off the handle. Became super angry for no apparent reason. The teacher wants to suspend him from school. I wish they would let him stay at school to help provide some extra support instead. He was really dysregulated’.
‘He likes to know what we’re doing, and how long things will take. That’s how he keeps himself regulated’
These are just a few examples of situations which can occur with those who interact with children or adults who struggle with regulating themselves. ‘Dysregulation’ occurs when someone has trouble regulating themself, and can be really hard for those who parent, teach, or care for those who struggle with this ability.
A new diagnosis, which has recently been named Disruptive Mood Dysregulation Syndrome, or DDRS was added to the DSM V when it was released in 2013. This diagnosis is a collection of symptoms that previously had not been captured under other diagnoses. Below are some examples to help explain regulation, and its partner, dysregulation.
History of Shared Characteristics and Diagnosis
These shared characteristics have been lumped in with Attention Deficit Hyperactivity Disorder, Bipolar Disorder, and Oppositional Defiant Disorder historically, depending on the clinician and the trends of the time period. In 2013, DDRS was added to and included in the latest Diagnostic and Statistical Manual, version 5 (DSM V).
It is what I have usually thought of as children or adults having intense reactions, sometimes referred to as temper tantrums. It also includes children who are sometimes referred to as ‘difficult’ or ‘bad’ or ‘hard to handle’ by their caregivers.
Those who meet the criteria for this diagnosis usually ‘ramp up’ very quickly. What that means is that they can become angry or happy very quickly. People with these shared characteristics usually transition quickly between emotions and can be hard to predict, which can be really hard for those with a much slower transition time for their emotions.
Those with these characteristics have difficulties recognizing some of the usual cues, or what I call ‘warning signs’ of emotions. Anger is usually the emotion that gets in their way, as their quick anger outbursts can be pretty tough on caregivers. This is particularly true for people caring for a quick transitioner who transition between emotions less quickly. One example of a quick transition is someone who is referred to as having a ‘hair trigger’ anger response.
There are children who are very hesitant to leave their primary caregivers, or who are very ‘married to their routine’. Someone is Is ‘married to their routine’ feels strongly about following structure and routine in their life. That child may not want to miss day care or school because that is their routine, or they may not transition well to going for the same reason.
Another example is someone who bursts out laughing quickly, is quick to smile, or has what we call a belly laugh.
One of the benefits in thinking of Health and Wellness, instead of separating the two into Physical and Mental Health, is it allows us to think about the positive characteristics or qualities of these tendencies that can be so frustrating.
Instead of thinking of the collection of characteristics as a disorder, I suggest we think about temperament and our ability to transition and be flexible. We all know people who struggle with changes in their schedule. Someone else, who is less regulated, might put much less value on their planned schedule.
That person can be referred to as flexible when thinking positively, or flighty for someone who struggles to see the value of this temperament. For someone who is quick to transition, a better offer coming along than their planned routine is hard to resist. Someone who brought their lunch and then gets invited to lunch is probably going to go to lunch when asked if they enjoy social eating.
Examples of Differences in Emotional Response
One example of quick transitioning occurred in a position I had where I frequently ate lunch with my peer, who was in charge of development and fundraising, and the executive director, who had the job to make those final, important decisions even when they were hard to hear. We frequently ate lunch together and processed what was going happening in our work, which included final decisions (executive director), making sure we had enough funds and donations (development/person in charge of marketing and fundraising), and thinking about how we run our programs to meet the needs of the population we were serving (that one fell to me). At one point, I had picked up lunch at Panera, which is one of my favorites, and was planning to eat alone. When I returned to the office my peer and my boss were just heading out to lunch. I put that lunch right in the fridge and joined them. Because of my temperament, I rarely bring my lunch to work. I know that I am likely to abandon it and eat something different.
This example demonstrates how much I value social eating, my flexibility to a change in plans, and my willingness to pay for lunch twice in one day, justifying that I’d eat it the next day or for dinner. I can remember dancing my way out to the car to meet them and our laughter that followed.
Providing Support-making a difference to those with whom we work
As we begin to think about how caregivers and services providers, including teachers and family, can help those who fall under the category of struggling with regulation, it is important to look at a few different ways to provide support to the people with some of these shared characteristics.
For children who have experienced trauma in some way, these trauma responses, or reactions to stress, vary depending on their temperament and their attachment since birth. Each child has different resiliencies, which refers to their capability to withstand stress.
A child who has a higher resiliency in a family with multiple children may have very few issues with regulating themselves following a disruption in their life or routine, while others in the same family have a very strong, easily visible effect.
There are also those who have what is referred to as the ‘sleeper effect’, meaning that they appear fine and without symptoms following the initial trauma, and later show signs or symptoms of the disruption. Children whose parents divorce may not experience their trauma symptoms of the divorce until they get into some type of relationship with their future loved one, which is usually around the time they start dating, or when it is time to make a commitment to their loved one.
An example of a teen who struggled with regulation was a teen I met with in the mid 90’s who had a parent who was deceased. My memory is that her mother had substance abuse issues and had died, and the teen had also received some consequences for using an illegal substance called methamphetamine. It is the first time I remember hearing the term ‘crystal meth’, so I learned from the teen a little about that specific drug.
She lived with her father and her siblings. She had experienced some pretty severe consequences for her substance use prior to when I met her, and desperately seemed to crave stability.
Knowing what I know today from a Protective Factors standpoint, I would say that the family had very few social connections. They were pretty isolated, with few friends. The father’s resilience, meaning his ability to function in times of stress, was lower than some, meaning that this stressor in his life was really affecting him negatively particularly as it related to his parenting.
He was at a loss for what to do to help his daughter, or parent his other children, to help them all get what they needed. His knowledge of child development was also low, which is not too surprising considering the time period.
He was probably not parented in a way that would help him prepare for the nurturing aspects of parenting, nor did he plan for being responsible for all of the tasks related to daily parenting.
This teenager is what is commonly referred to as the ‘identified problem’ in the family. She was the child acting out (not following rules), utilizing illegal substances, yelling and screaming at her father, yelling at her siblings, and not having school success.
She had what can only be described as temper tantrums, which again is the term that I use anytime someone is loud about not getting their way. It is also one of the prevailing commonalities in this diagnosis. My perception is that those who are less good at recognizing their initial anger signs generally are in less control of their anger when they show it.
Here’s a graph to help with this example:
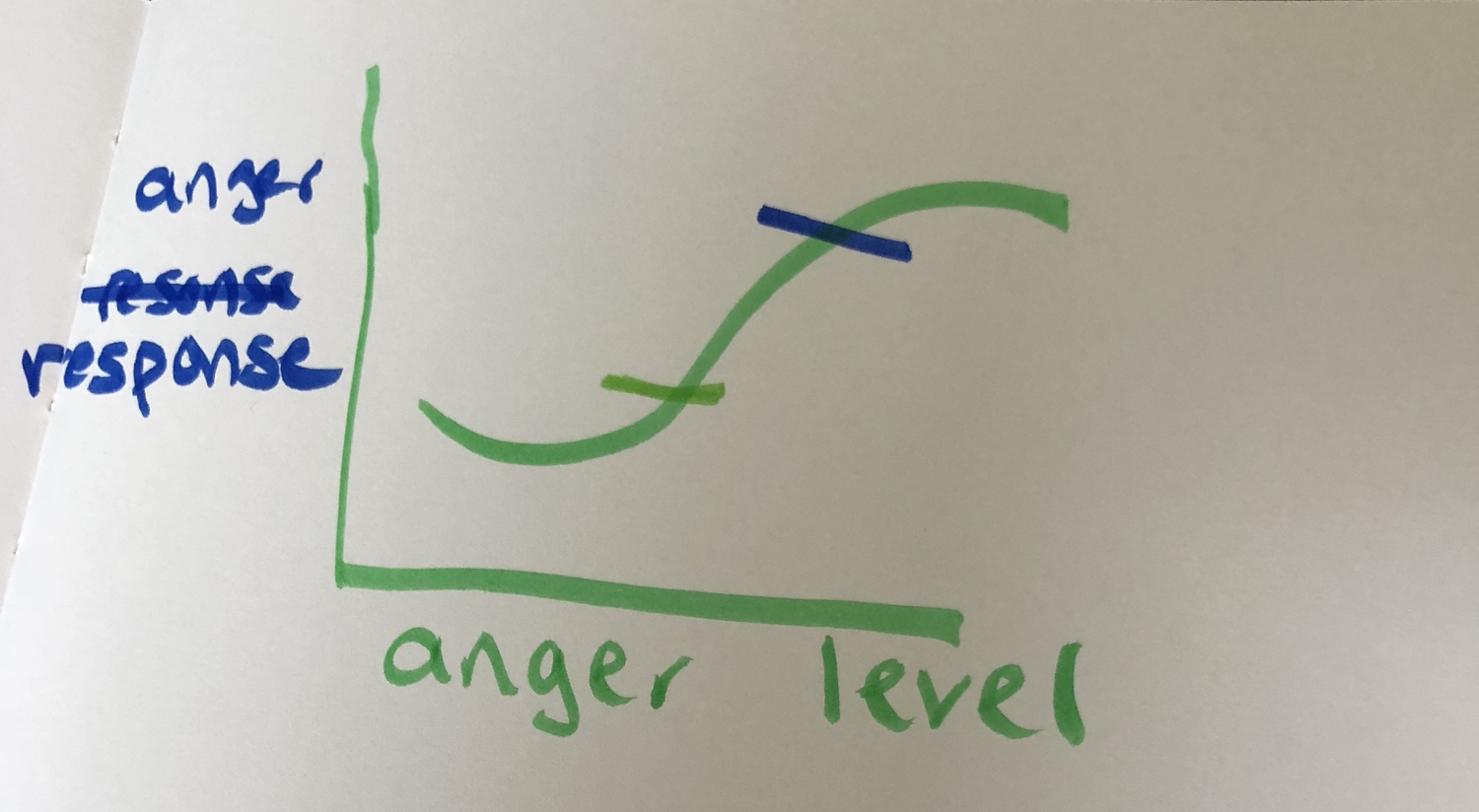
The graph above demonstrates our anger response and when we notice it. You can see that as the anger goes up side to side, , and as we go up and down looking at the anger response, the hash marks are where we tune in to our anger. If you notice your anger where the higher, green mark is, you are not in very good control of yourself.
The top hash shows someone who is pretty out of control. Yelling at people, maybe hitting people, doing things they receive consequences for, stuff that gets them in trouble.
The bottom hash, which is green, represents noticing, or becoming in tune with, anger much earlier. At that point, a person may notice their fists clinching, their face getting red, and their voice may become louder. The difference is, the person is still in control of themselves. They are still able to make better decisions about what they are going to do, or how they are going to behave, while being this angry.
As we work together, I encourage the child or adult with whom I’m working to make a goal of learning to recognize when they are becoming angry.
Personally, I have never met anyone who doesn’t get angry. Someone recently suggested Ghandi, but I’m pretty sure you have to be feeling pretty strongly to stage sit-ins and starve yourself to communicate your point. I’m going to go ahead and call that anger too.
My interpretation, in working with those at risk for being dysregulated and for those who become dysregulated easily, is that they are not very good at noticing their beginning stages of emotion.
We live in a society where, particularly middle aged adults, were socialized, as in parented, taught, and received messages on tv, not to show their anger. People who tend to want to please others really struggle with doing things that may or may not affect another person’s anger response.
We all get angry, we just don’t want to act in ways that have consequences like jail, kicked out of school, someone being displeased with us for some, or some other kind of consequence we perceive as punishment.
Strategies to Help…How do we Provide Support?
In order to work together with those who do not regulate easily, it is important to join together so that we are on the same page. Here are a few strategies I suggest for working together with those who are working to regulate themselves, and who may struggle with that.
- Work to recognize that some children or adults put a very strong emphasis on their schedule, while others put much less emphasis on that. It is important to respect the schedules of those who need their structure and routine, and to also realize there are those who do not need it as much. Those who need it less may step on the toes of those who do need it, not recognizing or respecting how important it is to ones who crave structure and routine.
- Communicate well with both children and adults about a change in schedule. What may seem like an innocent request to you may be devastating to someone who regulates themselves by that. Recognizing the effects that may occur from this disruption will help both the person who is regulating themself, and the person asking for the change in schedule..
- Work to give choice as much as possible. One of the reasons this has been diagnosed as Oppositional Defiant Disorder in the past is because of the very strong feelings that come with being told to do something without choice. Giving children a choice in foods they eat, clothes they wear, and other decisions can help with this change in routine, which affects regulation.
- Work on mindfulness techniques. Most people have a sense that they prefer to use to calm down. Some use music, some use things to look at it, for others it is sense of smell. Plan together, or figure out for yourself, which sense is most likely to help to calm down quickly, and develop a plan to do it. A song, looking at a lake or a picture of a lake, looking at a tree, or smelling cookies baking can all be things that affect this sense of regulation.
- Deep Breathing is the go-to technique that I teach to help with regulation. I also practice it in therapy. As I notice myself feeling agitated, or the person I am working with in therapy getting agitated, I will count to 4 breathing in, hold for 4, and release breathing out for 6. We repeat this sequence a couple of times as we meet to help get into the habit of recognizing when they need it.
- Checking in with others and self is another technique. When I feel frustrated or notice frustration with the person with whom I’m working, I’ll check in by asking ‘are you getting frustrated?’ This action helps put words to feelings, then practice a mindfulness technique giving choice about which one they use. This skill particularly works on 13–14 year olds, who have lots of feelings and not a lot of words to explain them.
Regulating emotions and techniques to help treat those with with difficulties in this area is an area that has room for growth. I am continuing to learn about what treatment approaches work with this population. It is exciting to begin to have some practices to address a set of characteristics that can be so hard to treat.


