You trust your doctor. Your doctor prescribed Xanax. It must be alright to take it, right?
Maybe not. Dr. Joanna Starrels, professor at the Albert Einstein College of Medicine, says “Generally speaking, primary care physicians have not received the training that they need to prescribe medications that have such high risk for addiction or overdose.”
Though psychiatrists prescribed benzodiazepines no more often from 2003 through 2015, prescriptions by primary care physicians during that period more than doubled, according to the Journal of the American Medical Association.
Why such an increase? Primary care doctors used to send patients with anxiety and panic to a therapist for Cognitive Behavioral Therapy (CBT). The feedback wasn’t good. Most patients found CBT did not end their panic attacks. JAMA Research confirmed what doctors heard from patients. Only one person in six treated with CBT became panic-free (“Usual Care Group” dark gray in the graphic below). When meds were added, the remission rate nearly doubled (“Intervention Group” light gray). The researchers advised, “Our intervention for panic disorder, a combination of CBT and antianxiety medication . . . resulted in substantially better outcomes than did usual care” (CBT).
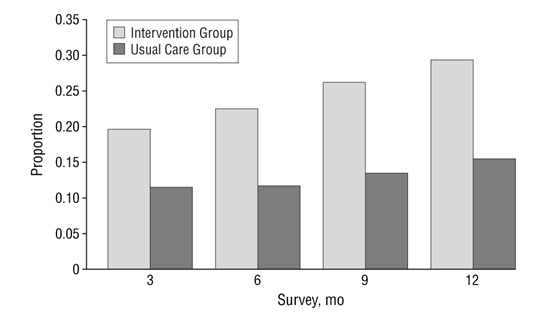
Source: JAMA Arch Gen Psychiatry. 2005;62(3):290-298. doi:10.1001/archpsyc.62.3.290
The study, published by JAMA in 2005, may have contributed to the doubling of benzodiazepine prescriptions by primary care physicians. Does a 13% remission rate increase justify the use of highly addictive medication? The study ended at 12 months. Over time, the 13% remission rate increase would most likely disappear. Dr. Anna Lembke, a psychiatrist, and director of addiction medicine at Stanford University, told CNN “People develop a tolerance, and they need more and more to get the same effect. The problem is in the long term, they lead to more problems than they solve,”
What does “more problems than they solve” mean? One problem is addiction. Benzodiazepines are notoriously difficult to withdraw from. To mitigate the risk of seizure, withdrawal should be supervised. A second problem is tolerance. When tolerance develops, the prescribed dose unexpectedly fails to control panic. In a state of panic, a person who is ordinarily savvy may take dangerous irrational action. For example, a fear of flying client told me she had flown for years using Xanax and that it worked well for her. But, without warning, she panicked aboard a flight. She took an additional dose. Benzodiazepines take time to work. When relief did not come quickly arrive, her panic increased and, frantic for relief, she turned to alcohol. She downed a few shots.
Alarmed at how casually she spoke of mixing Xanax and alcohol, I said, “Don’t ever do that. It’s dangerous. A person can tolerate a lot of alcohol alone or a lot of Xanax alone, but a moderate amount of the two together can make you stop breathing.”
“I know,” she replied. “I’m a nurse. But, I was desperate. All I wanted was relief.”
Unaware that she had developed tolerance, she boarded the flight fully expecting Xanax to protect her as it had before. During the flight, a full-blown panic attack took place. Overwhelmed, she was unable to think rationally. She reacted in a way that went against everything she knew as a nurse.
Tolerance sets an invisible trap. Dr. Lembke points out, “If they worked long term there would be nothing wrong with it, but they don’t and then they cause all kinds of harm.” Overwhelm occurs when meds unexpectedly fail to control panic. The frantic search for relief from panic after it has disabled the person’s rational thinking partly explains the rise in benzodiazepine-related deaths from 1,135 in 1999 to more than 11,537 in 2017.
CBT is unsatisfactory because of its low panic remission rate. Panic is not ordinarily a fatal condition. But, if benzodiazepines relied on for protection unexpected fail, panic results. Cognition is overwhelmed. The inability to think rationally places the person at risk of an unintended fatal overdose. Therefore, the use of benzodiazepines to increase remission by a mere 13% cannot be justified.
Fortunately, a satisfactory answer now exists. A panic control method developed in the SOAR fear of flying program is five times more effective than CBT. When applied to panic in day-to-day situations on the ground, it produces a remission rate of up to 87%.
Research Details
An email was sent on August 27, 2016 to 293 people who had enrolled in one of the SOAR fear of flying programs. The email was opened by 157 (54%) addressees. The text of the email is as follows:
To determine SOAR’s effectiveness in stopping panic, if you have time, please answer four questions. Just list 1, 2, 3, 4 and your “yes” or “no” answer and email your answers back.
BEFORE SOAR
1. Did you experience panic on the ground?
2. Did you experience panic in the air?
AFTER SOAR
3. Do you experience panic on the ground?
4. Do you experience panic in the air?
There are three SOAR programs. The full-length course consists of nine hours of instructional video and two hours of counseling by phone, The two condensed courses have three to four hours of video instruction and an optional thirty-minute counseling session.
Results Of The Study
Full-Length Course With Two Hours Of Counseling
- Results on the ground: 15 experienced panic on the ground prior to the course; 13 (87%) reported no panic on the ground after the course. One reported “small” panic, thus 93% became panic-free or improved.
- Results in the air: 21 experienced in-flight panic prior to the course; 17 (81%) were panic-free in the air after the course. One reported “less severe” panic, thus 86% became panic-free or improved.
Condensed Course With Counseling
- Results on the ground: 16 experienced panic prior to the course; 10 (50%) reported no panic afterward. Less panic was reported by 3; thus 81% were panic-free or improved.
- Results in the air: 28 experienced in-flight panic prior to the course; 19 (68%) were panic-free when flying afterward. Less panic was reported by 4, thus (82%) were panic-free or improved.
Condensed Course Without Counseling
- Results on the ground: 49 experienced panic on the ground prior to the course; 30 (61%) reported no panic afterward. Less panic was reported by 6; thus 73% were panic-free or improved.
- Results in the air: 61 experienced in-flight panic prior to the course; 41 (67%) were panic-free when flying afterward. Less in-flight panic was reported by 12; thus 87% were panic-free or improved.
Commentary
Though none of the SOAR Courses were directed toward alleviating panic on the ground, the intervention aimed at in-flight panic generalized to reduce panic dramatically on the ground.
The book Panic Free: The 10-Day Program to End Panic, Anxiety, and Claustrophobia adapts the method that controls in-flight panic to control panic on the ground. Accessible in book and audio-book form, the method can potentially increase the number of people who become free of panic as well as reduce unintentional overdose.
Readers who are good students, particularly if they are introspective, can get good results on their own. Some readers need to be guided by a therapist. The book includes an afterword for therapists written by Stephen Porges, Ph.D., professor of psychiatry at the University of North Carolina, past president of the Society for Psychophysiological Research, and recipient of a National Institute of Mental Health Research Scientist Development Award. Panic Free is based largely on his neurological research.
For too long, attempts to control panic have focused on controlling thoughts and avoiding stimuli that cause hyper-arousal. By discovering how our calming system, the parasympathetic nervous system, is activated, Porges made it possible to control hyper-arousal automatically. The method detailed in Panic Free, based on his discovery, has already enabled over 10,000 flight phobics to automatically control anxiety and panic.

