This piece was first posted on Substack. To comment, please go there.
The 1999 film, The Matrix, is about a man who discovers the world as we know it is actually an elaborate simulation created by intelligent machines who use it to control humanity in the “real” world—a dystopian future where the machines have taken over. In the decades since its release, the premise of the film has become an established metaphor for realizing that the world as it is can sometimes be radically at odds with the world as we perceive it. As one close-to-home example of this, I can recall the moment when I realized that health is more than doctors and medicines; that health is, in fact, an emergent property of the world around us, and that working to improve health means working to improve the context in which we live, and that it is that world that we should be focusing on to improve health.
Much of my career in public health has been an effort to make this very case—a vision of health that only sees health care is incomplete, that we need to talk about far more when we talk about health than treatment alone. In the post-COVID era, this strikes me as more important than ever. The dominant sense of the last 20 months is that what we just lived through was fundamentally a story about a virus. This, I would argue, is wrong, or at least incomplete. True, a coronavirus was the precipitating factor in what we experienced. But the nature of that experience was deeply, decisively shaped by the same factors that always shape health—politics, culture, the economy, the places where we live, work, and play, our social networks, and other structural forces that shape our world. Preventing the next pandemic means engaging with these forces, to shape a healthier society. To do that, we must first be able to see them clearly, to take the measure of their influence on health. Helping us do so is the aim of my forthcoming book, The Contagion Next Time, which will be released on November 1. The book argues that the pandemic was, at core, a story about how structural forces in our society left us vulnerable to the virus. The title is a tribute to James Baldwin’s book, The Fire Next Time, which helped readers better see the challenge of racism, and to insist this challenge must be faced in order to avoid future catastrophe. The Contagion Next Time aims to shine a spotlight on forces in our society that shape health by examining them through the lens of the COVID moment, and in so doing cast light on the world as we should perceive it, rather than the world that dominates in the public narrative.
Recognizing then that we need to see the world somewhat differently has me asking often, what is it that keeps us from seeing the right world? It seems to me that we see the world the way we do through our biases.
I would like to focus on three key biases that prevent us from seeing health clearly. For want of a clear label to these biases, I am going to call them our individualistic bias, our positional bias, and our sunk cost bias. It strikes me that it could be helpful in these weeks leading up to the launch of The Contagion Next Time to take a deep dive into these biases, so we might better understand the blind spots that can obscure what we talk about when we talk about health. This post, then, will be the first in a trilogy of columns looking at our biases, focusing today on the individualistic bias, and using as an example how we see the challenge of mental illness. I will talk about the other two biases in my next two weeks’ posts.
Let us then start then with the individualistic bias. It is probably easy for the reader to see the role this bias plays in shaping our thinking. In the US, our thinking about health is deeply linked to the individualism that characterizes so much of life in this country. We are continually hearing about all we can do, personally, for our health, from exercising to eating right. It is this bias that quickly distracts us from seeing the structural conditions that underlie health, and our responsibility to work, collectively, towards improving these conditions.
To illustrate how this bias works, let us take the example of mental health and our engagement with mental illness. For a long time, we did not discuss mental health the way we discuss physical health—that is, when we discussed it at all. Mental health—in particular, admitting to mental health struggles—was seen as taboo, a focus for stigma and shame. Happily, this has begun to change. This change has included a number of high-profile people opening up about mental health, from members of the British royal family, to athletes like Simone Biles and Naomi Osaka. All this helps inform a conversation where mental health is more and more seen as on par with physical health—as it should be.
But this evolving conversation, and its intersection with high-profile voices, has, in my assessment, been shaped by our individualistic bias, distorting our view of the issue. In this case, the individualistic bias pushes us to think that we are all equally vulnerable to poor mental health. The observation that prominent, wealthy, persons struggle with mental illness further accentuates this point (“if they can have mental illness, so can anyone”). And while it is indeed true that anyone can suffer from poor mental health, and we should have the compassion to recognize that, our individualistic bias obscures the fact that mental health is subject to the same socioeconomic forces that create disparities in physical health, making certain populations more vulnerable to disease than others. Money, housing, social networks, exposure to stressors—these factors all play a part in shaping mental health. Because access to assets like money and decent housing is more tenuous among the socioeconomically vulnerable, these populations are at greater risk of mental illness, particularly when crisis strikes.
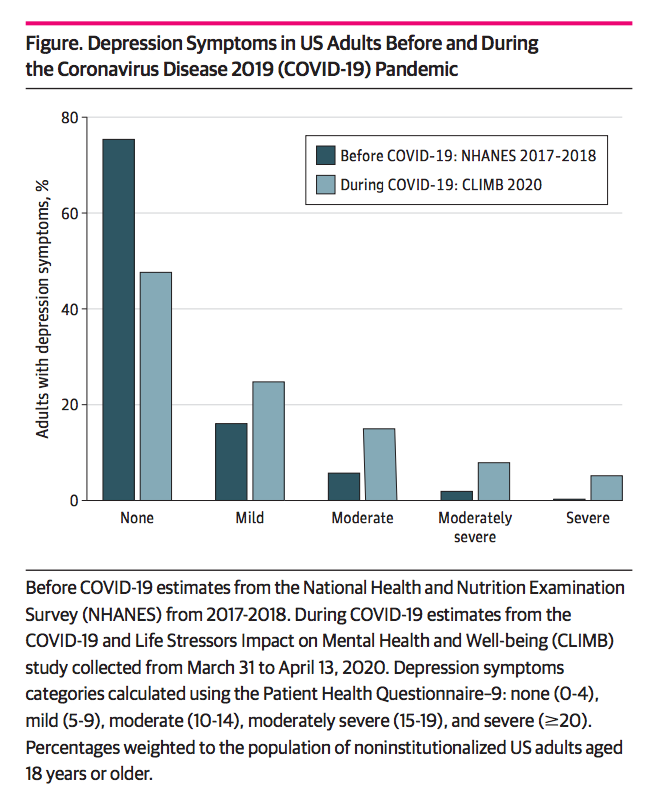
This was well-illustrated during COVID-19. Last year, I was part of a research team that found depression rates tripled during the pandemic among US adults. We also found that lower income, fewer savings, and greater exposure to stressors were linked with greater depression risk. This month, our team published the first year-long longitudinal study of depressive symptoms during COVID-19. The study was conducted on the same representative sample of US adults in the first study, having followed this group from Spring 2020 to Spring 2021. We found that, unlike after other traumatic events where depression tends to taper off in the long-term, depression during COVID-19 remained high. We also found that stressors such as housing, lack of childcare, and job-loss were all linked with greater depression one year into COVID-19.
In many ways, these data confirm what is common sense in thinking about mental health. Imagine, for example, a woman, Diana, who has long struggled to make ends meet, is working multiple low-wage jobs, but always falling behind. This burden, combined with the responsibility of caring for two children, and the challenge of living in a poor, unsafe neighborhood with few friends or family nearby to help her, caused her to suffer from depression. Now imagine her facing these challenges during the COVID-19 pandemic. Imagine she lost one of her jobs during the pandemic and could not find a new one. Imagine her fearing for her children’s safety and having to look after them at home each day during a year of school closures. Under these circumstances, it is no wonder that she might find herself suffering from a burden of depression that is deeper, and more prolonged, than what is experienced by people with fewer challenges in their life.
When presented in these personal terms, it is easy to see how socioeconomic context shapes vulnerability to poor mental health. It is also easy to see how such context can be overlooked in our conversation about mental health. Because people like Diana have fewer assets, less financial and social capital, they also tend to have less clout in the halls of power and less representation in the national debate about the issues that matter most to their health. This all suggests strongly that efforts to improve the health of all, consistent with our vision in public health, must be preceded by a moment in which the scales fall from our eyes, and we are able to clearly see the full range of conditions that shape health, beyond a narrow focus on doctors and medicines. And it means resisting the temptation to blame individuals for their poor health, as our bias towards individual behavior at the expense of context can cause us to do.
Our findings, reflected in the fictional story of Diana, suggest a reality in which vulnerability to poor mental health is deeply shaped by socioeconomic context. This suggests that when it comes to improving mental health recognizing that all of us are at risk of poor mental health is a necessary but insufficient step towards transformative change. Recognizing the ubiquity of poor mental health must be accompanied by efforts to address the conditions that leave certain populations disproportionately vulnerable to mental illness. This means that it is imperative to engage with mental health at the level of the forces that shape these conditions, particularly at the political and economic levels that do so much to shape access to the assets that support health. Such steps require us to look beyond our bias towards investing in health care alone and investing in creating the structural conditions that support health.
With this in mind, we can see how our bias against seeing the full picture of health might obstruct this engagement, complicating our efforts to address mental health. It would be easy to continue thinking that no population is any more or less vulnerable to mental illness than any other, and that the only factor shaping this vulnerability is the internal, mental state of individuals. Seeing the structure that truly underlies mental illness takes a willingness to look beyond what may seem obvious, to get at the roots of health. This means first acknowledging that we have biases, and recognizing where they may have led us astray.

