The latest iteration of U.S. Dietary Guidelines for Americans (DGAs) has been contentious to say the least. Since publication in December 2015, the guidelines have inspired passionate critique about their content and legitimacy from multiple camps.
To address criticisms and concerns, Congress reached out to an august, well-respected, independent body: the National Academies of Sciences, Engineering and Medicine (NASEM). NASEM now has a Congressional mandate to evaluate the entire process used to develop the DGAs, and NASEM has assembled a non-partisan committee to undertake the work.
As a fellow in NASEM, I expressed interest in participating in the committee’s work. However, criteria for participation included having no industry relationships and no prior public statements related to the DGAs. Given my recent advising for a food-product and cookware company, and my conspicuous past critiques of dietary guidelines in invited talks and published commentaries (like this one), my formal participation was not in the cards.
Nonetheless, I was fully free to participate in a public workshop that the NASEM committee hosted on January 10, 2017. The excellent presentations and comments from this full-day workshop spanned more than 8 hours. For those not lucky enough to attend, l will highlight some of the content (and controversies) here.
Overview in Nutrition
Presenters in the workshop discussed the subtleties of science and policy related to nutrition. The day began with the former chair of the 2015 Dietary Guidelines Advisory Committee, Barbara Millen, who explained her committee’s scientific work in the context of a socio-ecological model (considering individuals in the context of their social, cultural, physical, and policy environments).
High-priority topics that Dr. Millen’s 2015 committee undertook included food and nutrient intake, dietary patterns, dietary behavior change, environmental settings, agricultural sustainability, and food safety. The 2015 committee covered 82 separate research questions — about a quarter through systematic reviews.
Systematic review — comprehensive collecting and analysis of published literature in a transparent, reproducible, scientifically rigorous way — was a focus of much of the workshop day. Several government agencies and independent academics presented on challenges and nuances related to systematic reviews, particularly in nutrition.

Challenges of Research
For any scientific review, getting the research questions right is imperative (e.g., do fruits and vegetables work? How do fruits and vegetables work? What works better, fruits or vegetables? … or whole grains?). Elements of a good research question include the specific populations of concern (e.g., healthy adults? children? people with diabetes?), the specific intervention (e.g., low-sodium? plant-based? high-protein?), some comparison (i.e., the intervention relative to what?), and outcomes (e.g., blood pressure? avoidance of cancer? quality of life? longevity?). Often times, differing research-question elements between studies challenges arrival at a unified aggregate conclusion.
Even when there is a unified conclusion, one has to assess the uncertainty around it and then what is the “right” thing to do (e.g., low-carb? low-fat? … neither? both?). To prioritize questions, critical considerations include the burden of the condition to be avoided (e.g., obesity), the number of people affected (e.g., everyone in the US or just a subset), and the implementability, effectiveness, and durability of the strategy (e.g., of the DASH diet) … as well as competing options (e.g., Ornish, Atkins, Paleo).
Then there is the quality of the evidence to consider. One sobering presentation made clear that after more than a quarter century of looking, we are still trying to figure out how to measure dietary intake objectively (turns out our memories and our reports about what we eat are not all that accurate). And we are still trying to account for complex interactions in nutrition (people don’t eat individual vitamins or minerals in isolation, or even individual foods for the most part, we eat mixed dishes and food and drink in variable combinations — a very messy and challenging thing to study).
Advances in Methodology
To address some of the challenges, there have been advances. For instance, presenters discussed how “food pattern modeling” can answer “what if” questions, like what would be the impact on caloric intake and obesity if we all started making “nutrient-dense choices” (e.g. whole fresh peaches) vs. “typical choices” (canned peaches in heavy syrup)?
There was also discussion about how randomized controlled trials (the gold standard in clinical medicine and pharma) play an important role in nutrition, but are neither feasible nor appropriate for most nutrition research. After all, dietary patterns are complex (not simply take this pill or don’t) and there are issues related to blinding (you know if you are in the cheeseburger group or not) and compliance (people may have trouble sticking to a sprouts-only diet).
An alternative to randomized trials — or really a complement — might come from systems science. Systems science better measures complexity, capturing dynamic behaviors (e.g., carnivore today, vegan tomorrow), bidirectional relationships (e.g., fattening because you’re over-eating and over-eating because you’re fattening), non-linearity (e.g., eating chips up to the threshold where you start noticing your waist expand), and time-delay effects (ah, if only we could eat like we did in our 20s …).
The take-home quote I loved from the systems science talk was “all models are wrong, but some are useful.” That observation is true beyond systems science.
All Guidelines are Flawed. Some are Useful
Later presentations during the workshop day considered dissemination and implementation of the DGAs. While guidelines have provided the basis for research priorities and educational materials at the federal level, speakers discussed the problems of there being no validated way to align federal nutrition programs with the DGAs. Also, complying with daily and weekly requirements for school meals produced unintended consequences (like removal of truly healthful well-liked foods like guacamole and hummus due to a narrow focus on fat).
Invited speakers had a lot to say about the guidelines. So did the “public.” Rather, so did industry groups, professional societies, and non-profit organizations. The NASEM had put out a call for public input on challenges and opportunities with the DGAs, and special interests came out in force.
There were the Grocery Manufacturers Association and the American Frozen Food Institute, advocating for industry’s role in the DGAs, and the Physicians’ Committee for Responsible Medicine and Center for Science in the Public interest, advocating against it. There was Atkins Nutritionals arguing to cut carbs, and the American Bakers Association arguing to promote them. The Egg Nutrition Center promoted yolks, the McCormick company promoted spices, and The Institute for Food Technologies made a case for a greater food-scientist involvement. At least 4 organizations came out in support of breastfeeding.
But where was the voice of the people — actual identifiable people?
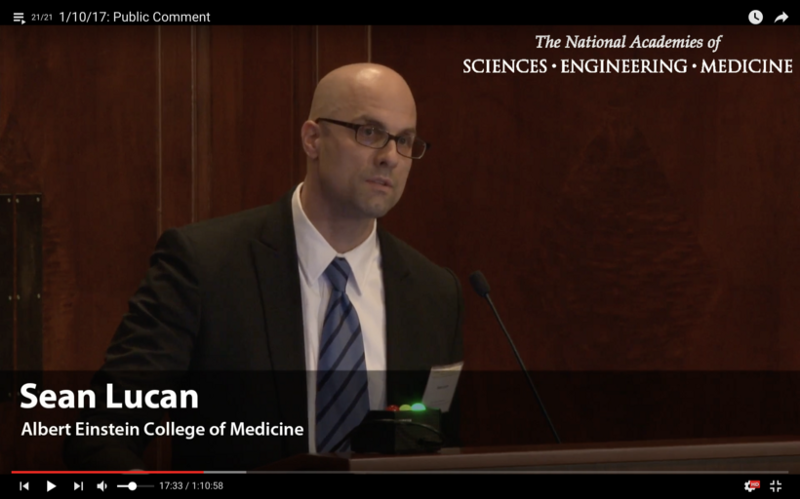
A Doctor Speaks
While perceived conflicts kept me from participating on the NASEM committee, I might have been among the least conflicted “public” representative in the room. Yes, I serve on the Scientific and Nutritional Advisory Board of a food-product and cookware company, but my goal in doing so is to support products and programs that improve the nutrition and lives of real people. My role as an advisor is to inform the company when their products are true (and when they are not) to a mission of healthy convenient eating.
At the NASEM meeting, I was not representing that company though, or any company or organization for that matter. I was representing myself, as a doctor, and representing my patients. I conveyed to the committee how physicians and patients struggle to translate esoteric guidance to healthful eating, and how much of the DGAs are not very culturally sensitive or inclusive. I also expressed concern for integrity in a process heavily influenced by industry. I emphasized that compromise of science, nutrition, and public health for lobbying, politics, and special interests is the biggest issue.
All guidelines are flawed, but they need not be dishonest and bent. Making guidelines truer to science, more culturally inclusive, and more user-friendly would truly be useful.
Sean C. Lucan, MD, MPH, MS Associate Professor of Family and Social Medicine
Originally published at www.huffingtonpost.com on January 18, 2017.
Originally published at medium.com


